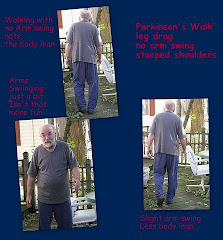
- Leg drag
- Lack of Arm Swing
- Loss of Sense of Smell - decreased sense of smell - phantom smells
- Changes in Handwriting
- Changes in Voice
- Change in Facial Expression
- Pain or achiness in the Shoulder or Neck, more common in women
- Depression, anxiety, stress
- Sleep problems - especially with especially with REM sleep or more specifically RBD sleep. Sleep issues may also include "acting out" during sleep: Yelling, kicking, punching.
- Signs of specific Vitamin Deficiencies: Ds and Bs especially
- Sharp small pains - pinprick pains - or perhaps small areas of numbness
- An odd type of vertigo - which may actually be Orthostatic Hypotension which is known to develop years before the actual PD diagnosis
- Dizziness
- Adding additional symptoms beginning 4-05-11 with THANKS to the folks at Patients Like Me
- Urinary issues such as urinary incontinence or frequency
- Impairment of color discrimination - may improve with levodopa
- Fatigue - tiring more easily at routine tasks - lack of stamina - daytime sleepiness
- Cramping
- Rhinorrhea - that's a runny nose to most of us
- Seborrhoeic dermatitis - an autononic symptom, an immunodeficiency - flaking is often confused with dry skin - possibly seen as dandruff
- numbness - usually in extremities
- We would like to learn if people experienced any of the following as precursor - earliest - symptoms
- Sleep apnea ?
- Constipation
- RLS - restless leg syndrome?
- Excessive sweating - an autonomic nervous system dysfunction?
- Personality changes or changes in Executive functioning
- Hyperhydrosis or excessive sweating which can sometimes appear as Seborrhoeic dermatitis - might feel like hot flashes
- Erectile Dysfunction
- Vision issues such as difficulty focusingI'd also like to add: Unexplained tripping or falling which I overlooked
- Investigate neurophysiologic tests that have the potential of serving as screening tools- New Haven, CT
- Consortium On Risk for Early-onset Parkinson's Disease (CORE PD) It is still recruiting at Columbia University, NY, NY and at Rush University Medical Center, Chicago, IL
- Developing hindsight: Biomarkers of Risk of Parkinson Disease
Our best body of knowledge now comes from proactive patients who share their stories. Not all are sucess stories but they demonstrate the importance of a the current studies and the importance of a productive doctor-patient relationship. Many thanks to those enerous folks on Patients Like Me who added to the list of early warning symptoms.
What we are wondering is whether the immediate treatments will lie more in Alternative Medicine in the form of Nutritional Supplements rather than in pharmacological medications. What will be the role of therapies such as Forced Exercise?
You might also be willing to contribute to the knowledge base by registering to participate in an NIH study:













I am a 56 year old female. My mother has parkinsons, diagnosed about 3 years ago. I am living with her and help her do chores and bath. I have been extremely tired. Neck aches, shoulder, I fell today, could not keep my balance, very afraid I WILL BE THE ONE WHO INHERITS THIS CONDITION. PLEASE ADVISE.
ReplyDeleteThe first thing anyone is going to tell you is that you are under considerable stress and are exhibiting those very symptoms.
ReplyDeleteSince your mother could be eligible for some in-home nursing care, this is the time to learn of those benefits and to make use of them.
You need some pampering as well. Perhaps medical massage would be of benefit for both of you.
But you didn't write about that, you are concerned that you have an inherited form of the disease and are manifesting precursor symptoms.
I would suggest that you and your mother make use of the PROGENI study for LRRK2
(you'll have to cut and paste this link)
http://progeni.iu.edu/getInvolved/index.asp
and
The 23andMe study which has already made progress in learning more about PD genes.
https://www.23andme.com/pd/
There is research in another method of lab testing for the presence of dopamine in the brain but that is years from completion.
Please keep a chronological journal of all symptoms, when they occur, meds and supplements you are taking so that you will be prepared for your doctors visit.
I know you are physically and emotionally exhausted but this is the time to take the best care of yourself for both your future and your mother's. If you have siblings, they need to be advised that you will need a few days off from time to time.
When you see your doctor you will beed to be proactive because you know that STRESS will be the first and only focus unless you are insistent. That doesn't mean the issue isn't stress but that doesn't mean it is the only possibility. You could have both.
Fallig early in not that common unless you have other signs of postural instability. Be prepared to explain that fall: how you were feeling before, how you fell, whether you had a cold or sinus infection or other ear problem also at the time. They'll start with blood pressure and go from there.
Our advise is to follow up on several of the suggestions we have made - don't just pick one.
I'm a 63-year-old woman. As you said, people could have many of these symptoms for a variety of reasons. What I wonder is if people who develop Parkinson's may have had these symptoms for decades before ever having something they might describe as Parkinson's and there may be clues that should be followed up on much earlier. I cannot remember when I was able to sleep without aid and usually have horrific dreams. I was born deficient in B vitamins. I've had neck/shoulder pain for years. I have always lived with depression and anxiety. I've had RLS in the past but not currently. All of those things are easily attributable to other things. I have difficulty focusing, which I've been attributing to my astigmatism. As you wrote, any time I've gone to a physician about problems, his answer has been "stress." Now both arms, but particularly the left, are having tingling and numbness. I also notice that when I hold a spoon it seems fine until I bring it to my mouth and then it begins to shake. That started me looking online and I saw this post. Only one of my 8 aunts had Parkinson's, and my mom did not; however, I'm thinking this may finally be the time to pursue this.
ReplyDeleteJust diagnosed with pd. had rls for years and tingle in left arm for over a year.
DeleteSince there is no cure for RLS, it could be that those symptoms are under control.
ReplyDeleteBecause PD is actually a collection of syndromes with varying symptoms and rates of progression, it makes sense to pursue further diagnosis both to rule out conditions and to focus on a diagnosis which will lead to effective treatment.
Are you tested regularly for vitamin deficiency?
PD tremors are usually at rest tremors as opposed to the action tremor you describe. Actually some of the symptoms you describe do sound like B12 and B complex deficiency.
Are you treating the anxiety? Behavioral therapy? Counselling? Medication? Supplements? Yoga or Tai Chi?
What an eye opening article! I cannot believe, I put in the medication I was on, and it brought this up. I have not one of the symptoms you listed, but ALL. They have danced MS with me for years, then said NO, your just under too much stress, of COURSE I AM, I AM A FEMALE ...right? It is funny, I watched a very old episode of a TV show recently, where just this thing occured. The lady went to the DR, she was in pain, tired and just felt bad, his answer: Your under stress. He sent her home dismissed as an over emotional female. Not long after, she went back she saw other Doctors until she found out...she had breast cancer. I am weary of the attitudes of Doctors. I will add one VERY IMPORTANT factor here, that EVERY WOMAN SHOULD DO:
ReplyDeleteGO GET COPIES OF YOUR MEDICAL FILES!!!!! You will NOT believe what some phy. write about you, even those you THINK are you friends...they arent! Thank you for this input....and good luck to ALL!
Enlightened!
My husband, 50 yrs old, is concerned about PD. His grandmother had it and he feels he has similar symptoms. He had a stroke (TIA) 7 yrs ago and recently had a radical prostectamy for cancer. He has tremers every now and then in his Rt hand /arm when he eats and for the past 7 yrs, he loses his balance quite often. Within the past yr he's complained about sore, stiff legs and has had rls for yrs. He has also complained about numbness in the back of his head off n on. He says this is what his grandmother went through during the early stages. When he explained it all to his pcp ...he was immediately referred to a neurologist. He is also on weekly vitamin d2 for almost a yr now.
ReplyDeleteMy husband, 50, has recently become concerned about PD. His grandmother had it and he doesn't know any health info on either side of his family. He had a stroke (tia) 7 yrs ago and just this past March, a radical prostectamy for cancer. He takes vit d2 once a week, is diabetic (dr says it's under control) complains about numbness in the back of his head, rls, has tremers in his Rt hand at times while eating and loses his balance from time to time (getting worse) while walking. When he explained this to his PCP, the dr didn't hesitate to refer him to a neurologist.
ReplyDeleteI was diagnosed with hypoKalemia or potassium deficient only 5 months after giving birth to my daughter who is now 12 yrs old. When it gets worse, I can't lift my arm much less walk without falling down so I crawl. I am still on medication - kalium durules. whenever my condition gets worse, doctor would order that I get KCl drip until my K+ level goes back to 4.0. Year 2009, I had bell's palsy and I thought was cured after therapy but from time to time my face still gets deformed as described by my family. My smile isn't the way it was anymore. Lately, I have been experiencing numbness in my right hand particularly all fingers. I went to my doctor and was told my K+ level is okay at 3.0. I am currently taking both my potassium meds and b-complex. Is it possible that I may have early signs of PD? what tests are necessary to find this out?
ReplyDelete
ReplyDeleteIn 2008 I strted having numbness and tingling on my right side along with the following - no more multitasking, bored easily, depressed, not able to sleep, and at any moment I wanted to fall asleep. I had MRIs, CTs, etc... and they ruled out MS, Bells Palsy, Lupos and treated me for migraines. Continued having problems bt finally gave up and lived with i.
2010 it started bothing me lot again and now I has weakness in my right leg but the neuro I went to told me I needed to see a shrink. There was nothing wrong with me in 2008 and there wasn't going to be anything wrong with me now.
Now it is 2012 and I am again trying to figure it out. I have the same numbness and tingling but I now have a tightness in my right side - arm, leg and sometimes torso. I also get very weak on the right side. 2 weeks ago I had a very sharp and extremely painful pain in my right shoulder followed by the tightness. It would come and go and at times I would also have numbness and tingling in the arm, leg and face. This lasted for a week. A week to the day of the first sharp pain I was hit again. The same type of pain shot from one shoulder to the other and up my neck. After it was over and I tried to speak I was copletely hoarse. Later I became so week on the right side I could barely use my arm or leg. The next day I went to the hospital. I stayed the weekend and the did the usual, MRI, CT, bloodtest and found nothing. I am now seeeing a nuerologist but he is treating me for migraines but my symptoms are not going away.
I have been reading up on Parkinsons and I would like to list my symptoms and see what you think.
I get what we call "episodes" where I go completely limp and feel like my muscles dont want to work. During this I breath weird and sould like I am on some crazy drug.
Started with a twitching finger (it gets very tight and I have a hard time moving it) and now have it in my hand and foot. All on the right side.
Numbness and tingling, tightness, weakness in right side.
One toe on my right foot will go completely numb sometimes.
I get a horrible pain in my neck. It is a tightness and I catch myself trying to pull my neck to stetch it but it doesn't help.
I notice that I hold my arm close to my side because it is so weak/tight and sometime limp because my leg is so weak.
I do not sleep well. I wake up every few hours and I have violent nightmares. I wake up yelling and I catch myself before I hit my husband.
This summer I noticed that I was sweating more than usual. I thought I might be going thru early mentapause but I live in Miami and everyone I mentioned it to said "no, its just hot outside"
I have to keep changing deoterant because I will start to smell even if I haven't been sweating alot.
I always have tons of hair fall out but my hair is not thinning.
My hair has become very oily. My hair has been dry my entire life and now it feels like I need to wash before dinner.
My face has become very oily and it was not oily before.
I am constipated but I have been most of my life.
I often have problems getting words out properly. I will usually stop and wait and later I will try again.
Right after the pain shot from shoulder to shoulder and up my neck I started wanting to swallow alot and the other day I took my son to the movies and fell asleep while there. I woke myself up becasue I was choking on my own saliva.
It has not happened often but I have noticed that I lose my balance at times.
And the newest symptom started yesterday when both sides of my jaw tightened and it felt like I couldn't open my mouth. I didn't tell anyone it happened and when I tried to answer a question from my son he replied with "Mommy, are you faling asleep? You sound funny" He told me that he could barely hear me and I was talking very slow.
What do you think?
Btw, I am a 39 year old female and I do have PD in my family but it is my 2nd cousin.
Well dear u sound like u have really suffered with this & one things 4 sure - if u have gotten a dr. that tells u go c a shrink & u KNOW this is very real & not in ur head --- then get urself another neruro --- & get as many as it takes until u find one thats on the ball!! I went thru EIGHT in 2 yrs & finally found ONE that was able 2 help me! AND IM A NURSE!! So I've been there with those that tell u theres nothing wrong & those that tell u maybe u should consider seeing a shrink bc its in ur head & it if was hard for ME 2 find a gr8 dr. then I know it cant be easy for the
Deleteaverage person out there thats not in the medical field!
So u just dont give up!! But one things FOR SURE!! U dump those docs u have tried in the past & KEEP DUMPING THEM until u find one thats on board with u!!!
And also - try an Endocrinologist along with the Neuro just 2b sure ur
hormones r right & theres no pituitary trouble. And dont take it from any other specialist but an endocrinologist about ur pituitary & hormones - blood test results can be tricky when it comes to hormones.
And oh - may sound weird but sometimes weird things can do weird stuff so get urself checked 4 lyme disease. It may not show up in regular bloodtests if uv had it 4 a long time & being that it all seems to be on one side u'd think it wouldn't be lyme - but I've seen that stuff give
ppl CRAZY symptoms!!
I hope u feel better! And sleep is 2 important! Get meds if u have 2 for sound sleep bc sleep helps ur body heal....=)
So do whatever u have to do to get GOOD SLEEP! Even if it means taking a med to get it!!! Just remember to alternate ur meds about every 6 to 9 mths bc u do not want 2 build any tolerance to any sleep meds esp. one that works gr8 4u!!
DeleteHugs... =}
tight feeling around the chest sounds like MS. MRI will eventually maybe show this.
DeleteA tight feeling around the chest could be a symptom of a number of conditions. Have you seen your doctor?
DeleteThat symptom of tightness was a symptom which Steve had before I took him to the ER where he was admitted and had an angiogram where 3 blockages were found. They did the angioplasty on only one artery, the one with 90% blockage. I always wished they could have addressed the artery with 60% blockage as well.
The point is, have someone drive you to a doctor immediately. Prepare a written chronological list of symptoms on the way.
BTW, my father also had that symptom and cutting to the chase, his heart stopped before the quadruple bypass surgery and twice in the operating room.
Steve had the angioplasty a handful of years before his PD diagnosis but angina was the one symptom which was not related to PD.
I'm a 45-year old female. Doctors have been trying to find out for some time why I am having various problems:
ReplyDelete*my hands go numb, my arms and hands tingle
*I am always tired
*I feel little tremors in my hands like they are shaking inside my skin
*smells drive me crazy
*I can't remember words and struggle to concentrate
*I don't sleep well and have crazy dreams
*I am perimenopausal
*random sharp headaches in the temples and forehead that don't last long
*dull headaches that won't go away
*neck and shoulder pain
*jaw snapping while asleep
*constipation and diarrhea
*cold extremities
I take thyroid medicine and Vitamin D supplements. I have clinical depression and take Zoloft. I stopped menstruating at the age of 43 and I've taken both estrogen and progesterone supplements. I've been to a physical therapist to try to relieve the tingling and numbness and neck and shoulder pain. I've had a colonoscopy. I use oxygen when I sleep but it doesn't seem to help. I wake up gasping for breath. I'm having hot flashes.
These symptoms may just be random things but what is really bothering me is that my hands feel like they are shaking inside, and I can see them shake sometimes. Mostly though I just feel it. My father died of ALS and I've had other relatives with dementia and related tremors. I'm hoping I'm just generally unhealthy and a hypochondriac.
What do I even do to find out? What tests can detect PD once it's started?
Dear Anonymous,
ReplyDeleteOne problem with a multi-symptom situation is that we often see the specialists for each separate symptom. Have you been to a neurologist with your entire list?
Some of your symptoms could be related while others might not. My guess is that you are hoping that some of your symptoms are stress related and yet several point you in a few other directions. Diagnosis may require a neruologist, an endocrinologist or another specialty but since you already know there was ALS in your family, please begin with a good neuro.
While the genetic results for ALS are not in yet, it is known that in some cases, the earlier the onset of treatment, the longer the lifespan.
And don't be afraid to return to share the results because they will most certainly add to the knowledge base as well as the discussion. And because we care and want to know how you are doing.
Hi im 36 year old female and ive had right hand tremor for 4 years but now has gone to my thumb and pointy finger.....i have tremor in right leg ,my muscles ache and have trouble getting out of chair and trouble rolling over in bed....my neck is always sore and i clench my jaw all the time,i have pin prick feelings in legs sometimes and feel tired all the the time .....i lose my balance and my hand writing is very tiny.....my hand cramps up wjen brushing my little girls hair and aches and wen im upset or its very hot my tremor get worse to the point i have to hide it.....i get burning in right foot and have a limp that comes and goes and wen ppl are talking to me its like my mind is on something else and i have to say sorry what did u say????could it be parkinsons
ReplyDeleteI was diagnosed w PD in 2001 at age 47. Some symptoms I had before 2001: depression starting in my 20s; head injury about 1984 w loss of consciousness, had been a knee bouncer/jiggler most of my life until PD really set in, constipated for as long as I can remember, urination problems too, excessive muscle tone/tightness; my gait was a distinctive "step-clomp, step-clomp;" my lips were asymmetrical; faded color vision, esp. w red; tried cocaine a couple of times and I felt nothing. Two years before diagnosis was very deeply depressed; felt like I was walking through knee-high mud; held my right arm in a spastic posture; developed an action tremor in right hand. The only test I know of is they give you some carbidopa/levodopa pills and if you feel better, congratulations, you have Parkinson's disease. Luckily for me, I felt so much better after taking the piils, I wasn't that depressed about having PD; the pills had completely erased my depression which had not been helped by any of about 10 antidpressants. Now, about 15 yrs later, my symptoms are much-changed and life is very difficult. Considering DBS surgery.
ReplyDeleteIs knee bouncing (not restless legs) an early sign?
Is lack of response to stimulant (cocaine) significant? Seems to me that lack of dopamine results in lack of addiction. Smoked for a while but could easily drop it (social/weekend smoker); caffeine does nothing for me; I have never uttered the words I love food or I love to eat.
I have read that constipation and depression are early signs; also that PD may start in the gut somehow, then travels up the vagus nerve into the brain. Yikes!
Knee bouncing as well as constipation (and diarrhea) can be a response to stress. The body is acting out or releasing stress in this way. But inability to deal with excessive stress can lead to depression as the anger turns inward. However, your response to carbidopa/levodopa suggests that you probably had early onset or YOPD for years. Other People with Parkinsons will have to tell you if they also experienced knee bouncing as a precursor symptom. Consider asking that question at a Patients Like Me PD forum page.
ReplyDeleteAt Drugs.com you can read:
Cocaine’s effect occurs in the midbrain region called the ventral tegmental area (VTA). Neuronal fibers from the VTA connect to the nucleus accumbens, an area of the brain responsible for rewards. Animals studies show that levels of a brain chemical (neurotransmitter) known as dopamine are increased in this area during rewards. Normally, dopamine is released and recycled in response to these rewards. The use of cocaine can interfere with this process, allowing dopamine to accumulate and send an amplified ‘reward’ signal to the brain, resulting in the euphoria described by users. 1.
National Institute on Drug Abuse (NIDA). NIH. Research Report Series. Cocaine: Abuse and Additiction.
Note that in Parkinson's disease the concern is with dopamine in the substantia nigra pars compacta.
As to the origins of PD in the body, you are correct. There is current research which is pointing to the gut.
http://www.lunduniversity.lu.se/article/disputed-theory-on-parkinsons-origin-strengthened
https://www.michaeljfox.org/foundation/news-detail.php?gut-check-on-parkinson-new-findings-on-bacteria-levels&smcid=smcid=ag-a30U00000004dnS&gclid=CNftrrfpo8cCFQoLaQodMokJsg
http://www.medscape.com/viewarticle/842705http://www.medscape.com/viewarticle/842705
How is your sense of smell? Diminished ability to smell - the first sign of pleasure (along with sight ) when eating can affect your sense of taste. The result is little enthusiasm about eating. Since this was a problem in our household, I tried to color balance as well as strongly season. It helped. There might be a link to the gut origins and sense of smell as you have probably read.
Keep us informed if you decide to have DBS for your motor symptoms
In looking over the list of indicators, it's interesting that I showed signs of these things prior to 2005, but wasn't diagnosed until 2010. People around me would ask one another if I had health issues, but did not ask me. After heart surgery in 2011 my wife began to see markers and was prompted to look into it further after seeing a news report on TV. She called up the site online and measured my actions against the questions asked. I hit on 6 or 7 of 10 markers. The neurologist watched me walk, asked about how I felt and listened to my response. "When I wake up sometimes it feels like my whole body is quivering." We had an MRI and ultimately wound up on Azilect and Mirapex.
ReplyDeleteI try to stay up on developments and look for trials. I read more and share what I find.
One diagnostic issue is that the early symptoms are often seen individually. Column A, Column B and so forth but never as a combination plate or a family dinner.
DeleteSteve's symptoms began more than 5 years prior to his diagnosis as well. And yes, he saw doctors for several of them individually.
Patients probably need early on training as well as medical journals. Of course, that makes us all sound like hypochondriacs but if we don't, who will know our real medical history and how things add up. Steve's doctors actually had his entire chart every time they saw him for a "symptom" but they probably didn't have time to review.
We've said it before - patients need to be proactive and also to share with their families. Thank goodness for your wife, she's one smart cookie!
The thing we need to do, collectively, is let others know about our condition. I wrestled with that one since I don't like to publicize things, but this one is different. Family and friends need to understand why we struggle with walking, dressing, eating, and doing chores. We need to get past self pride and tell of our limitations and frustrations. We need to tell one another where to find PD friendly clothes and shoes and things that make life a little easier. And we need to share, share, share about support groups, breakthroughs, etc. We aren't victims unless we choose to be.
ReplyDeleteAmen to that. If you circle the wagons, the enemy will be within. Not only do friends and family want to support you, they want to assist in meaningful ways. They are also excellent observers and can help you with information you convey to your doctors.
ReplyDeleteI was a healthy, normal 29 year old but developed orthostatic hypotension. It took a while for the cardiologist to realize it wasn't an issue with my heart and he referred me for a tilt table test to confirm the suspicion. I started treatment and returned to a normal life of being a busy, active person. Four years later I began dropping things with my left hand and then my leg started dragging. I started tripping when trying to walk onto the curb or up steps. Fatigue became common place. I only have weakness progressive on my left side. EMGs and MRIs ruled out things like ALS and MS. They diagnosed it as neuropathy (I still have feeling but reduced circulation in my leg leg/foot). My grandfather had PD. I do not have a tremor but my left arm is contracted and in a fist. I thought my body did it for balance but it just sort of stays there when I'm walking. I haven't met a lot of folks with Parkinson's and am wearing AFOs and using an arm crutch for balance help. I'm curious if anyone else has any experience with young onset PD and if this looks like that? I've seen two neurologists at home and they're stumped.
ReplyDeleteI don't know where home is but it sounds as if you need a neurologist who specializes in motor disorders. You don't need a tremor to have PD or one of the related neurodegenerative conditions.
DeleteIve had RLS and heat intolerance..all my life..Tremors in high school were notice by my keyboarding II instructor when she noticed a sharp decline in my performance from 400+ words per minute with 0 error..She called the school nurse as I felt "out of it"...They chocked it up to possible blood sugar problems that were ruled out...And I just ignored it ...Urinary retention was an issue during delivery of my oldest child, when repeated insertions of the catheter didnt seem to work....Hyperhidrosis began to be extremely bothersome at age 21...Looking back, I remember being called "clumsy K" because I tripped a lot and all my left shoes had scuffs, from what I realize now was an obvious leg drag..The extreme muscle cramps in the neck and upper back (AKA dystonia) began at age 16..dystonia and leg drag became more frequent and visually noticeable to others (looked like a bodybuilder) after I had my last child at age 25...( Stress definitely increases symptoms)...at age 30, After my sister passed suddenly and my husband became more abusive, EVERYTHING came to a head and the "stroke like" symptoms hit me all at once..leg drag, turning in of my left foot, stuttering progressed to loss of speech, and vision issues, memory/cognitive difficulty,(not knowing why I was at the store or how I got there)...Etc...after several Dr visits, and being told I was just "stressed"...(my children were more independent by this point...so, I knew deep down, it was something else...After I lost my ability to drive...I finally went to an ER and the Neurologist there was amazing,....He saw more and observed me for several months...Treating me with a small dosage of sinemet, which seemed to make my life normal again...In December, 2012, 4 days after my 30th birthday, after he consulted with his partner in the practice, a team of experts at our University neurology Dept I was given a diagnosis of young onset Parkinson's...It was such a relief, however, I still needed to know I wasn't "crazy"..So I went to a Movement disorder specialist at UAB hospital and saw a Dr who didn't know my full history,for another opinion.. and immediately was diagnosed with Young Onset Parkinson's with full body dystonia.
ReplyDeleteThank you for sharing your history with everyone. Your symptom record serves as a progressive guideline.
DeleteOn a personal note, I hope that you no longer have to endure an abusive situation at home because you have been a real heroine who went untreated for so long.