Depression is a common problem for many people - we hear those ads on television every day along with the side effect warnings. Parkinson's patients, their families and caregivers alike may go through periods of depression. The remedies and treatments for PDer and the carer may differ because of medication and supplement interactions and the disease itself.
Some research has indicated that the chemical changes in the brain caused by depression might actually be a trigger for PD. We know that Parkinson's shows itself after a significant loss of the neurotransmitters dopamine and norepinephrine; is serotonin deficiency occurring at the same time or earlier? One view is that synaptic depletion of serotonin allows a fall in norepinephrine levels. Which might mean that manipulating serotonin levels would increase norepinephrine levels if the norepinephrine depletion hadn't occurred because of the dopamine depletion. Which is why depression treatment can be different in Parkinson's disease.
Depression is often one of the 1st symptoms of PD - long before any obvious ones. Older patients can also manifest confusion, memory loss and apathy. PD is not the only disease associated with depression; Alzheimer's disease, kidney failure, stroke, AIDS, chronic fatigue, fibromyalgia, cancer and hypothyroidism patients also suffer from depression.
The PD symptoms for depression range from lack of energy, a struggle to arise to begin the new day, sleep disturbances, feeling irritable and anxious, have a sense of the loss of self-worth, feeling of self-guilt and loss of appetite. Because depression often manifests early it may seem to everyone that it is an extension of the appearance of Parkinson's Disease symptoms and the diagnosis. The depression may come and go. In the late stages depression may actually be caused by a chemical imbalance.
It is understandable that people would be depressed by having any disease because there is the shock, the grief and the sometimes not so subtle physical changes. There are differences in PD. A primary difference is that the depression over loss of mobility and appearance of other motor symptoms may actually acerbate the symptoms.
Psychological therapy such as cognitive-behavioral therapy as opposed to psychotherapy can be of benefit to PD patients because it can help restore a more positive self image which can assist in improving caregiver and family relations as well. It can also help the patient focus on problem-solving rather than the loss.
There are also medications which help. Be aware, however, the Cleveland Clinic information suggested that amoxipine (Ascendin) can make PD symptoms worse. And there are others which can cause low blood pressure. Selective serotonin uptake inhibitors (SSRIs) are among the more recent, safer meds. However, recent a study showed that nortriptyline, a tricyclic antidepressant (TCA) which targets both serotonin and norepinephrine receptors was more effective in PD patients than paroxetine (Paxil) an SSRI. Tricyclics are older antidepressants which must be monitored closely for overdose
If you are taking Zelapar or Zydis selegiline, Eldepryl, Cipro (Ciprofloxacin) there are cautions about taking antidepressants, SSRIs and tricyclic antidepressants because of interactions and side effects. Prozac and Zoloft may cause anxiety, tremor and insomnia.
Much to our surprise, we read that electroconvulsive therapy ("shock" therapy) works more rapidly than medication and may actually help improve other PD symptoms in some cases.
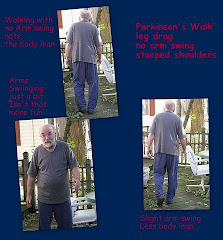
Another important treatment is exercise. It will help both the the depression and the PD symptoms.
There are also supplements which can help. Remember that medications are not the only substances which can cause side effects. Food and dietary supplements also have side effects.
Most of us are familiar with St John's Wort. You can also find St John's Wort in combination with 5-HTP and vitamin B-6. L-5-Hydroxytryptophan crosses the blood brain barrier and is said to help relieve anxiety and depression as well as being a natural relaxant which also aids in insomnia. There is some evidence that 5-HTP should not be used with carbidopa. If you are taking Azilect, if you are combining with MAO1 inhibitors, you should make sure to consult your doctor before taking ST John's Wort or 5-HTP. (Currently Teva, manufacturer of Azilect, is working with the FDA to change the description to MAO-B inhibitor which can be more broadly prescribed.)
Because of the impact upon the three molecules, the big 3 monoamines of Parkinson's, it is important to discuss any supplements you are considering with your neurologist. Melatonin is another supplement which is used in low doses to treat depression because it is known to raise serotonin levels and to help adjust the sleep cycle. Supplements should not be taken without a discussion with your physician.
It is important to keep in mind that everything you take into your body, including the foods you eat, will interact with everything else you take. Some combinations are synergistic, they work well together and may amplify the benefits while combining others can cause serious side effects.
One last area to discuss is Seasonal Affective Disorder - SAD.
It isn't just the winter blues because you feel cooped in even when you have to go out and about. SAD is more serious than that. It affects patients and caregivers alike. Some people have SAD even in the spring and summer.
We'll talk more about SAD in the next post - better late than never.













No comments:
Post a Comment
Welcome to Parkinsons Focus Today.
We are delighted to hear from you by comment here
or through email as found in Contact Us.
Please do not include email addresses if leaving a comment online.
Email addresses are used only for email responses.
Spammers take note: your messages will not be published. The comments section is for an exchange of ideas, not for backlinks.