.jpg) Introduction to Questions about Parkinson's Disease
Introduction to Questions about Parkinson's Disease
Earlier this week we received some questions from a student who was working on a project for school. Since it's easier to create a questionnaire when you already know the answers, we've revised the question list and are presenting it here with the introductory remarks we also provided.
Introduction Please understand that this patient is only in between phase 1 and 2 and hopefully with the help of the medications he is taking and the addition of supplements and physical-type therapy, we will be able to hold the PD where it is now for awhile. You should know that each patient will manifest symptoms in a slightly different way; certain symptoms may never appear in some patients. Some patients progress rapidly from stage to stage.
Advanced stage PD patients might not be able to answer your questions. At that point you might need to talk to the caregiver and even they might not be able to answer precisely for obvious reason that they are not in the mind of the patient. By this time dopamine levels in the brain have fallen so severely that the remaining neurotransmitter cells cannot function well enough to prevent contracture of the limbs and sometimes the torso. This is more common in patients with psychosis. At the advanced stage the dopamine auto-receptors do not seem to be functioning much if at all.
Another thing you should know is that there are usually undiagnosed precursor symptoms - symptoms which appear well before the standard identifiable symptoms of Parkinson's disease. These symptoms are not identified by either the patient or the physician as being disease related. One school of thought on this is that as the dopamine and subsequently the norepinephrine cells die and their neurotransmitting ceases, the limited dopamine resources are allotted to other body functions. Sense of smell, an early symptom, may be seen by the brain as being peripheral and therefore reduced or shut down.
Depression is another precursor symptom. Being depressed by having the disease is logical but having the depression or severe stress can be either a trigger or an early symptom. PD depression is not treated successfully in the standard ways because the source is different. There are no standardized test for dPD but there are existing depression tests which can be used.
Since Parkinson's, long thought to be an idiopathic disease, may actually be a genetic disease which can skip many generations until it responds to a trigger or a built-in trigger on a mutated gene - there are several associated with PD - it is commonly an older person's disease. The numbers of patients go up at each year over 65. There are also young-onset or early onset patients who manifest differently in many cases. Their response to meds are different also. And sadly there are also juvenile PD patients whose symptoms can manifest between 2 and 20 years of age. The last two groups have not received nearly enough attention in the past.
There are different courses of treatment for patients as some prefer to postpone levadopa medications in favor of levadopa agonists or diet, exercise and supplements. Many of the medications have side effects either short term or within a few years that impact a decision for that line of treatment. There is also some surgery which is about 50% effective in reducing the need for medication. Other courses of treatment include diet, natural supplements and types of physical therapy including exercise therapy, dance therapy, yoga, breathing, voice exercises, swim therapy and massage therapy.
Without these extras Steve's body would have stiffened far more than it has already. His massage therapist commented to him that she had never felt shoulders as stiff as his. We are working on that outside the therapy because without regular attention (once a week is not enough but certainly all that we can afford.) I perform a different procedure than the therapist. I was shocked the other day (the day before massage therapy) when his shoulders felt more like a car bumper than what shoulders should feel like. So I improvised and it helped. I did what was intuitive although contrary to what is recommended but it seemed to make a positive difference. I pulled back on his shoulders and then pushed forward against his shoulder blades. Next I moved his upper arms. I would like to say "gently" but it was not gentle. I raised both arms to touch his ears and then alternated with pulling the shoulders forward and back. I also deeply massaged the muscles on either side of his spine followed by moving his upper arms again.
Within the next week we will be making another video of him walking outside (we need space for this) so that we can compare it to videos we made 3 1/2 years ago. Because he also has arthritis in his knees, especially on his weak/stiff side, that has had a profound impact upon his resistance to that pain. The same options for arthritis treatment on knees available to the average person with arthritis are not viable options for a Parkinson's patient.
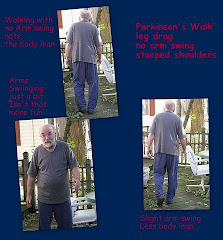
We have designed other exercises to assist his balance and leg stiffness which affect his ability to walk normally. PD patients often shuffle rather than being able to bend all joints in a normal walk. He has to practice turning by lifting his legs rather than pivoting which aggravates pain in his arthritic knees. We also work on his breathing and his voice. We work on shoulders, arms and arm swing. Again, if you read some of the blog articles or look at the photos, you can see the symptomatic posture with lack of arm swing, difficulty sitting and walking.
He also takes several supplements about which we have written before. He takes CoQ10, Turmeric, Nettle Root, sublingual Glutathione, vitamin B complex, a multivitamin with almost no iron or other heavy metals, slippery elm and fenugreek and a few others. Some of them are obviously helping. For one month we added a zinc ascorbate with vitamin C to help restore a bit of his sense of smell...which it has. He won't take that again for another month or two because taking for longer is contraindicated.
TOMORROW: The Questionnaire
Followed by:
PD Tests - The progression scales
.jpg) Introduction to Questions about Parkinson's Disease
Introduction to Questions about Parkinson's Disease












I finally found someone speaking about the complication when having PD and arthritis. I have pd and Rheumatoid arthritis and I cant seem to get the neuro. team to understand that my body is already crippled before being diagnosed with pd. I hope you write more about it. Especially the exercise part because I don't know what to do about that.
ReplyDeleteSyl,
ReplyDeleteWe think that if you check Patient's Like Me in the Parkinson's Disease community you will find there are others who also have PD and RA. You can register at no cost and ask a forum question or join in existing discussions.
Start printing all the material you find and give these pages to your doctors. We have found that many docs hear better with their eyes.
Ask your neurologist and/or your rheumatologist to write a prescription for exercise therapy. Make sure that you go to the best center around. We've found that those exercise therapists often have an excellent understanding of your body and can, through observation, provide you with an excellent course of exercises.
We would also suggest the best heated pool for aqua-therapy as you need low resistance exercises and balance therapy which water will provide. (Some pools are not kept warm enough)
In our area there is one center which has both exercise and swim therapy. I believe they now have massage therapy as well. Medical massage is very important for you as well.
You need range of motion, stretching, strength, aerobics. Do not confuse flexibility with flexing. You need stretching to achieve flexibility. One way to begin is Yoga to serve both medical conditions.
Do your doctors have any idea how much additional pain you suffer because of the PD coupled with the RA?