The Search for Motility along the PD Alimentary Canal
So even though we don't like talking about constipation, let's do just that so that we can do something about it.
What's normal? For some people 3 bowel movements a day can be normal - for others 1-2 times a week is normal but probably not a good thing because anything over 3 days allows for water to be absorbed followed by hardening of the stool. This hardening makes it even more difficult to pass the fecal matter. Medically 3X a week is necessary for the alimentary journey.
Hard stools can result in an anal fissure which is a painful tear which may be apparent by the blood on the toilet paper. When this happens regularly the spasms during defecation can push the hard stools against the wound and prevent healing. At this point you probably need to consult your doctor about how to handle the pain, the tear and softening of the stool.
It may be too late to remind you but men who have constipation are 3 times more likely to develop PD. Although this is no secret as it has been observed for almost 200 years, the Hawaii study confirmed it.
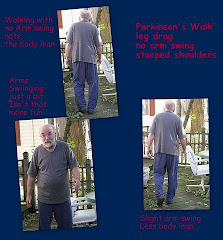
So why does constipation become an issue in Parkinson's disease which is often considered a motion disorder when the skeletal muscles just can't get the right messages? We know that skeletal muscle is under conscious control but smooth muscle is not under voluntary control nor is cardiac muscle. If the nervous system is not working properly, both smooth and skeletal muscles have difficulty in functioning as designed. Gastrointestinal (GI) dysfunction is the most common "non-motor" symptom of Parkinson's disease and the results of one small familial study indicated that it occured in about 60% of patients.
Add to that problem the fact that PD meds can also impact - quite literally - the GI tract creating that unpleasant situation of gas, bloating, nausea and general feeling of discomfort. Medications including antacids with calcium or aluminum and especially narcotic pain meds can contribute to or cause constipation problems.
Urinary issues can cause insufficient fluid - especially water intake - although caffeine and colas may have the opposite efffect. Many people
drink water as a constipation aid. Try warm water, perhaps with a bit of lemon.
Low fiber diets are a contributing factor: Fiber or roughage is the indigestible carbohydrate in plant foods. Fiber is either soluble or insoluble. Soluble fiber absorbs water and becomes gel-like as it passes through the body while insoluble fiber adds bulk to or softens stool but remains unchanged. A few insoluble fiber sources are whole grains, nuts, potato skins, cauliflower, zucchini, celery, the thick skins of some fruits, wheat and corn bran, often in cereal form. Soluble fibers include the fruity insides of apples, pears, bananas, berries, sweet potatoes, onions, broccoli, carrots, legumes. High fiber diets may also increase the bioavailability of levadopa.
Do not fail to
exercise regularly - and not just any exerise but exercises which target the abdominal and pelvic area. Kegeling is a good one for urinary issues and anal stimulation if done properly but may not be as effective as
Yoga breathing exercises and some simple seated bending over one leg and then the other. You can do this one lying down by bringing one bent leg as close to your chest as possibly with your hands clasped in front of you knee.
Just have the problem with travelling? Many people do irregardless of their health. For others it may be a high intake of dairy products can cause problems. We've learned that an unbalanced white rice-type gluten free diet can be problematic - but that diet just needs tweaking - much to our relief. No matter the cause, be cautious about relying upon laxatives.
So what will you do? Well there's
Bowel Retraining or Biofeedback. This begins with cleansing the entire waste removal system, including the colon, to begin to re-train the bowels to remove the waste products naturally. There are some high quality bowel cleansers out there. Just remember that an enema which acts as a bowel stimulant or a glycerin supository is only effective in colon. Some people take flax seed oil.
There are
medications such as Miralax; Zelnorm (
Tegaserod); Metamucil or psyllium, a bulk-forming fiber laxative meant to be used occasionally. Others take Domperidone, a peripheral dopamine antagonist which does not cross the blood brain barrier and appears to be effective for the upper GI tract.
When you talk to your doctor, be proactive. Constipation is another Parkinson's symptom, this time of the autonomic nervous system. You need a healthy plan of action to maintain quality of life and your doctor shouldn't just dismiss it as if it were a muted commercial on TV. You and doctor must distinguish between Acute and Chronic Constipation. Prolonged constipation in a Parkinson's patient is a serious condition; Medical personel should treat it seriously.
We'll talk about GERD, IBS, Celiac's and PD another day.
Resources and Additional Reading:
Biofeedback effectiveness clinical trial NCT00869830 has been completed but no study results appear to be available
Pilot Study information 2005 - revised - in pdf format You are not alone - lists a variety of constipation issues
Currently recruiting clinical trial for use of Amitiza/Lubiprostone for PD patients with Parkinson's at Baylor College of Medicine in Houston, TX and University of South Florida in Tampa, FL
Amitiza: is a chloride channel activator. It increases fluid secretion in your intestines which increases intestinal muscle movement and helps make it easier to pass stools (bowel movements). Amitiza is a chloride channel activator used to treat chronic constipation in adults. It is also used to treat irritable bowel syndrome in women with constipation as the main symptom - it works by increasing intestinal fluid and movement to help stool pass, reducing the symptoms of constipation. It can be used from 6 to 12 months.
Some Meds which can cause constipation
Narcotic pain medications such as codeine as in Tylenol #3; oxycodone as in Percocet; and hydromorphone known as Dilaudid
Antidepressants such as amitriptyline (Elavil) and imipramine (Tofranil)
Anticonvulsants such as phenytoin (Dilantin) and carbamazepine (Tegretol)
Iron supplements
Calcium channel blockers such as dilitiazem (Cardizem) and nifedipine (Procardia)
Aluminum-containing antacids such as Amphojel and Basaljel

















my dad has bad bowel probs but docusat seems a good help compared with senacot to mild
ReplyDelete