This is the first article I have written for my blog in almost six months. After eight years of having Parkinson's disease and treating it fairly successfully with medication, alternative medication and nutritional supplements, exercise, massage and diet changes, I ran into trouble between Thanksgiving and Xmas last year. I thought they were symptoms of PD.
The urinary symptoms which had been under control were no longer controllable; perhaps because I was neglecting to take the herbals which had helped for so long. Suddenly I had to urinate really frequently and didn't always make it to the bathroom even though my bed is only 20 feet away. I became afraid to leave home for fear of being too far from a rest room. Vivid dreams occurred so often that I could not tell what was real and what was not. My overall memory of this period is vague but I felt as if I were dying.
Although I primarily stayed in bed, often I thought I was someplace else and worried about how I was going to get home. In an amazingly short period of time I went from the early stages of Parkinson's to an advanced state; it seemed to take 2 or 3 weeks. (Editor's comment: it was practically overnight)
Even the open MRI which I was supposed to have done years ago, did not take place because it was too stressful for me. This doctor suggested that we could begin with an Xray and take it from there. He gave me the lab order but I was too shaken by the mere mention of an MRI to do even that.
We made the neurology appointment as suggested and then my wife decided that the Xrays had to be done before that appointment in three weeks. She finally nagged me to the lab for the Xrays a few days before I was to see the neuro. That weekend I hardly slept and the urinary issues were getting worse. I wasn't eating as much and had been limiting my coffee and tea intake because of the urinary frequency and urinary hesitancy. As a matter of fact, I was limiting all fluid intake. No fluid - no urinary frequency - no problem. But there was a problem and the frequency urges did not stop.
By the time we were talking to the neurologist, the transition was taking place. I asked not for the intended alternative treatment but for Sinemet which I thought would help the urinary issues. He agreed after the routine PD testing. By the next day the nightmare was developing full force.
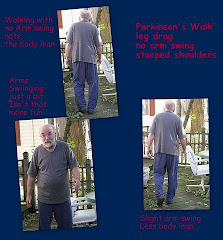
Almost overnight I was having difficulty walking down the hall. I could barely stand erect. Cognitive skills were muddled by hallucinations and illusions. I needed assistance to get into bed, instructions just to roll over. I needed help pulling up the blanket. Dressing and bathing without help was impossible. I would get up to eat but continued to drink only enough liquid to swallow a pill. I recognized the woman who prodded me about drinking more water during the day as being very similar in appearance to the woman who responded to my nightly hollering for help. Who was she? This nurse gave me my wife's name when I asked. What was this place?
My wife, meanwhile, was learning what you need to do to get a doctor's secretary to relay the seriousness of a condition. Because I had signed a release allowing the office to speak to my wife about my care, she knew she was on safe ground there. Her early calls were partially successful. The primary care office called back to refer her to the neurologist. The neurologist called back to say that Parkinson's disease can't go through such a short term transition and so we were looking for another cause possibly a UTI...and referred her back to the primary care doc.
She made the appointment for the following Monday and sat down to think and to discuss the issue with the massage therapist when she called to cancel my appointment. Sleep deprivation was only part of the problem. So she gave me cranberry capsules insisting that I drink more water. For half a day, I had a return to normalcy. And she had an insight. I was dehydrated.
When we went to the doctor's appointment, she took my urine specimen along. She insisted that it be tested. When it came back negative the discussion turned to prostate issues. We left with sample bottles of Flomax. What we didn't know was how long it would take before the Flomax would work - that it actually would be another 5 weeks before for the compulsive insistence that she walk me to the bathroom every 20 minutes would stop.
The dehydration issue was caused by the enlarged prostate which I knew about but didn't discuss much. Years earlier I didn't want to take the meds and had found relief with herbals. But this time I had confused the prostate problem with PD which exhibits the same symptoms. I'm an older man, older men frequently develop prostate issues. Had I talked to my new doctor about the problems instead of accepting that they were part of the disease, I wouldn't have had to endure all of this. The damage done by the dehydration, the stress for all of us except the cats - the dogs were very subdued during the first month - was intense.
It has been a long recovery and we learned a few lessons and revisited a few others.
















I'm really happy to see that you have finally written down what happened over the winter. I know that this information will be very valuable to someone out there in the future. Believe me, this was very frightening to more than just the dogs - being 900 miles away while this was going on was difficult.
ReplyDeleteIt was scary here also until we understood the problem and the resulting additional problems. Once I knew what was happening as a gestalt, I felt relieved. Then it became a matter of time.
ReplyDeleteI was most concerned by the lack of interest from the doctors' offices. While the neuro liked the mental challenge, he actually referred us back to the primary care doc's office.
Neither one would have taken action if I hadn't been insistent. But I admit, I felt really stupid when I realized that it was a prostate issue which caused the incontinence and the reaction to that was to dehydrate but not be forthright about it.
As a caregiver, one really needs to be on top of everything and I had let that slide because I hadn't read about prostate problems.
Also as a caregiver, I should have but didn't have any extra emotional energy for others such as yourself who needed reassurance and were entitled to it.
I'm glad to be on the other side of those weeks now.
Congratulations on having dodged a bullet. Any PWP who finds themselves in a "death spiral" like that must immediately rule out the PD and start looking fast before the medical profession takes control. As you found, dehydration is less a problem with water and more one of electrolytes, which can take one out of the game quickly. Another possibility is, as you mentioned, a UTI. Still another that is often overlooked is a hidden abscessed tooth. Infection means inflammation which, in the brain, means activated microglia churning out cytokines. And cytokines are neuroactive, i.e. they act as nerotransmitters and things can spin out of control quickly.
ReplyDeleteRick,
ReplyDeleteYou are right about the UTI or other infection as a possible cause. That was the first thing the neurologist suggested and the first thing we eliminnated with the primary care doc.
You make an excellent point about looking for other types/causes of infection. That should have been done and wasn't. There should have been an order for a simple blood test to look at the white cell count for starters.
Yes, Steve dodged a bullet because we did that pinch and lucked out. But the recovery took a long time and was not 100%.
I would have appreciated more and better professional help on this one.